Why healthcare providers are turning to offshore RCM teams
Healthcare providers are grappling with an uncomfortable irony: while medicine keeps advancing, the administrative side keeps getting heavier.
Claims take longer, denials keep rising, and staffing qualified revenue cycle professionals has become its own full-time job.
That pressure has pushed organizations to rethink how they manage their revenue cycle, and many are finding relief through offshore RCM teams.
These teams aren’t just a cost-cutting tactic. They’re becoming strategic engines for accuracy, speed, and long-term sustainability.
Here’s why the shift is happening and what makes offshore RCM teams such a compelling choice.
How do offshore RCM teams work?
Offshore RCM teams are dedicated groups of trained billing and coding specialists based outside the U.S., typically in top BPO destinations such as the Philippines.
They perform the same essential tasks as onshore teams, namely:
- Insurance verification
- Coding
- Claims submission
- Follow-ups
- Denial management
- Payment posting
The difference is that it achieves these with an offshore operational structure that delivers efficiency at scale.
Most providers integrate offshore RCM teams directly into their internal workflows. That means they use the same systems, follow the same KPIs, and communicate with the same level of accountability.
Rather than operating as a separate vendor, high-quality offshore RCM teams function as an extension of your in-house staff.
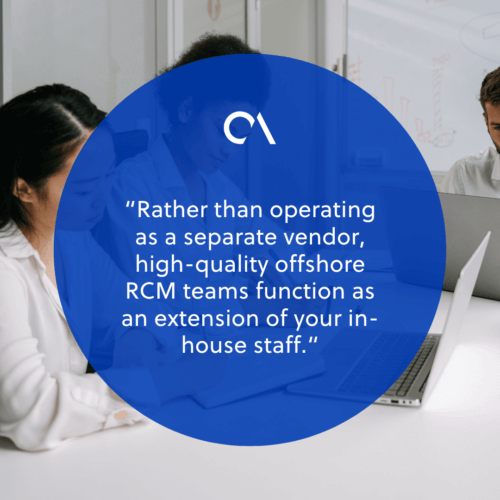
And yes—they work while your team sleeps. It’s not uncommon for providers to see their claims processed, backlogs cleared, and denial appeals already in motion by the time their local teams clock in.
But offshore doesn’t mean off-standard. Reputable teams are trained in U.S. billing regulations, payer requirements, and evolving coding standards.
Many of these offshore staff have backgrounds in healthcare administration or billing certification programs. This gives providers instant access to specialized RCM talent without the lengthy hiring and training cycles.
What’s behind the shift to offshore RCM teams?
The move toward offshore RCM teams didn’t happen because healthcare providers suddenly wanted to experiment with new models. It happened because old models stopped working.
Staffing shortages
Staffing shortages are at the top of the list. The demand for skilled billers and coders far outweighs supply, and turnover continues to stretch teams thin.
Every vacancy slows revenue cycles, increases denial rates, and forces existing staff to take on more work—often burning them out in the process.
Operational pressure
Operational pressure is another driving factor. Claims complexity has skyrocketed. Payer rules change constantly.
Even the best internal teams struggle to keep up with tightening reimbursement rules and mounting administrative tasks.
Financial strain
And of course, financial strain plays a major role. Hiring and retaining in-house RCM talent is expensive, especially for small and mid-sized providers.
The American Hospital Association has called out “skyrocketing” costs in hospital administration. Findings show that over 40% of expenses are incurred in delivering care, while around $40 billion annually is spent on billing and collections.
When payroll, benefits, and overhead keep rising, it’s no surprise that providers explore ways to maintain quality while reducing costs.
Offshore RCM teams solve all three issues: access to talent, operational stability, and financial predictability.
Benefits of using offshore RCM teams
Healthcare providers wouldn’t be adopting offshore RCM teams at this pace if the benefits weren’t compelling.
Here are the biggest wins organizations report:
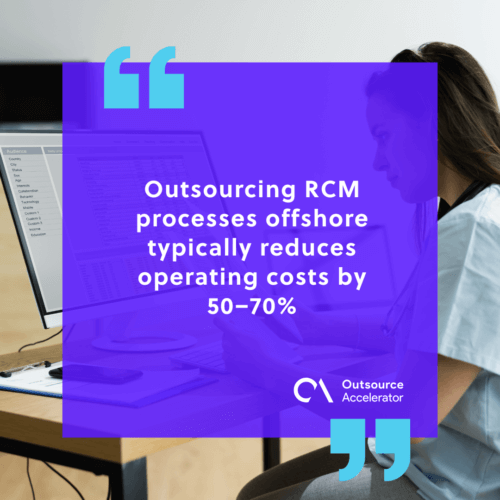
1. Cost efficiency without compromising quality
Outsourcing RCM processes offshore typically reduces operating costs by 50–70%. Because these teams work on dedicated models, providers get specialized support at a fraction of the cost of expanding in-house operations.
2. A deeper, more reliable talent pool
According to the Change Healthcare 2022 Denials Index, the initial-submission denial rate for claims hit nearly 12% in 2022, up from around 9% in 2016. This highlights the danger in having in-house staff take on the added burden of RCM.
Offshore RCM teams offer immediate access to billing specialists, coders, denial management experts, QA analysts, and insurance verification teams. All of these professionals are trained in U.S. healthcare processes.
This eliminates the painful cycle of recruiting, hiring, and replacing talent.
3. Faster claims, fewer denials, and smoother cash flow
By processing claims continuously, offshore teams shrink turnaround times and help stabilize reimbursements. Their specialization also leads to fewer errors, stronger coding accuracy, and better follow-up performance.
4. Built-in scalability
Providers can expand or streamline their offshore RCM teams based on seasonal needs, growth stages, or fluctuating patient volumes. This offers flexibility without the financial risk of hiring new full-time staff.
5. 24/7 operational momentum
While onshore teams rest, offshore teams keep the revenue cycle moving. This improves throughput, reduces backlogs, and ensures no day is wasted waiting for work to resume.
Why Connext is a trusted offshore RCM team partner
If you’re evaluating offshore RCM teams, choosing the right partner makes all the difference. Connext Global Solutions stands out for delivering highly skilled, HIPAA-compliant offshore RCM teams that operate as a seamless part of your organization.
Connext recruits experienced medical billers, coders, claims specialists, and RCM analysts trained specifically in U.S. healthcare workflows. Their teams integrate directly with your systems, follow your SOPs, and maintain the accuracy and accountability your revenue cycle demands.
With secure infrastructure and strict adherence to compliance standards, Connext ensures protected health information stays protected—full stop. And because their model focuses on dedicated teams, you get continuity, strong retention, and a stable workforce you can rely on long term.
If you’re ready to improve billing accuracy, accelerate collections, and scale with confidence, Connext can help you build a custom offshore RCM team designed around your goals.
Reach out today and start transforming your revenue cycle operations with a partner you can trust.







 Independent
Independent




